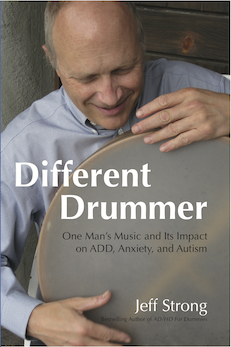
by Jeff Strong
Strong Institute Director
The following is an excerpt from my book, Different Drummer: One Man’s Music and Its Impact on ADD, Anxiety, and Autism.
I could hear the screaming as we pulled into the driveway. I looked with concern at Lloyd, who simply raised an eyebrow.
Knowing they were expecting us, Lloyd and I walked right into the house and were immediately confronted by Ty who was running through the entryway screaming and flailing his arms.
His mother was following behind, trying to catch him.
Lloyd motioned for me to set down the drum and grab a chair for him as he took stock of the situation. Then he sat down behind the drum and began playing.
He started with a loud slap to the head. The drum’s shout filled the huge room and reverberated off the hard surfaces, drowning out Ty’s screams. Lloyd paused then gave the drum another hard slap.
Ty turned to look, but continued screaming, hitting and pushing his mother away as she caught up to him and tried giving him a hug.
Lloyd tapped the head with the tips of his fingers, laying down a soft patter that was barely audible in the midst of the chaos in the room.
Once out of his mother’s arms, Ty made another lap around the room then came running toward Lloyd and grabbed at the drum. Lloyd was unfazed and kept playing, holding the drum between his legs as six-year-old Ty pawed at it.
Ty’s mother took advantage of Ty’s focus on Lloyd and the drum and was able to get a hold of him. Ty squirmed, but didn’t put up much of a fight as Lloyd raised his volume and began playing in earnest.
I was still stunned by the difference in Ty’s behavior from the last couple of sessions with him. This was our third meeting with Ty; and although Lloyd had told me before we met Ty that he was prone to aggressive outbursts, I hadn’t seen one yet. The Ty that I had observed up until that point was a quiet boy who was intent on occupying his own world, generally oblivious to everything around him. The screaming, running, and lashing out where new to me.
These behaviors, however, were something that I became intimately familiar with in the following decades.
I thought of Ty’s screaming and physical aggression as I entered the yard of the residential facility where I was getting ready to conduct a study. Located in a rural area not far from where I was living in Arizona, this home for adults with autism had been profiled in a newspaper article. I called the home, hoping to be able to play for the residents. Only a year before, I had seen the remarkable calming effects of one of my tapes when it was tested at an adult vocational center. (I talk about that research project in Chapter 9). I was told that this facility was having troubles with its residents’ anxiety and aggressive behavior; I hoped to make customized recordings for each resident to see if my drumming could help.
Once through the entry gate, I saw a man coming toward me. He started yelling obscenities as I approached, his pace toward me quicker than my pace toward the administrative office. I started to say hello and ask him where the director was, but he simply continued on in great detail about how he was going to hurt me—punch me in the face, kick me in the groin, elbow me in the chest—if I crossed him.
This was Charlie, one of the residents and one of the reasons I was at this facility.
His threats were directed to me at a high volume and without making eye contact. By my observation and experience with other men with autism, I didn’t feel that he really intended to act on his threats. He had the characteristic monotone, lack of eye contact, and overall flat affect that characterizes many with this condition. He also lacked the usual intensity and in-your-face aggressiveness that typically precedes such an attack.
Nonetheless, given his history of unprovoked aggression, I was careful not to get too close or to upset him if I could avoid it. I did, however, sit down on the bench near the garden and pick up my drum, which he regarded curiously, and begin to play, which prompted him to watch me even more closely. I was pretty confident that he had never encountered anyone entering his space and drumming. The novelty of this situation seemed to disarm him, because he stopped talking and watched me.
I began by quietly playing calming-type rhythms at the characteristic REI eight-beats-per-second pace. Over the next few minutes, I slowly built up the volume of my drumming and before long he sat down next to me. A few minutes later he put his hand on the shell of the drum.
After approximately four minutes, I began a series of more intense rhythms to see if his behavior would change. This is what Lloyd used to do to invoke a response in a listener and to gauge their level of engagement in the rhythms. Within less than 30 seconds, Charlie grabbed the hardware lugs that tension the drum and tried to pull the drum from my lap. Because I have become accustomed to anticipate a reaction of this sort (I’d lost hold of the drum many times before), I pulled back and just barely managed to hang on.
After a short struggle, he let go of the drum and leaned away from it, though he stayed on the bench. Using the calming-type rhythms I started with, I began playing again. He settled back on the bench. I continued playing for another ten minutes or so, careful to not play rhythms that were too intense or chaotic. He noticeably calmed during this time and was sitting still, gazing off in the distance as I stopped playing and walked away.
Charlie’s response was not unlike Ty’s when Lloyd finally got into a groove. With his mother’s arms around him, Ty stood holding the drum as Lloyd played. I stood in awe as Ty was drawn into the pulse and power of Lloyd’s drumming. Lloyd played for almost ten minutes and all the while Ty stood and held the drum. Ty was calm and allowed his mother to hold him by the time Lloyd stopped playing, so we decided to call it a session and leave.
When we got to the car, I asked Lloyd what he did to calm Ty down.
“I hit the drum with intensity to get his attention. The first slap didn’t do anything. So I played another,” he described.
“That’s when Ty looked at you,” I said.
“Yes, but he was still out of control. I needed to do the unexpected, so I played exactly the opposite way next. Instead of yelling, I whispered.”
“I could barely hear what you were playing. What rhythms were you using?”
“Nothing special. The whisper was the important thing. He needed to search for the sound.”
“And he did. He came right over to you. It was amazing.”
“He was still out of control, though.”
“Yeah, I noticed you switched rhythms or something. The sound was so, I don’t know, pleading.”
“I was talking to him. Asking him to join me. To surrender his violence.”
“Then he just stood there. His mom held him and he didn’t move. Why did that happen, and so fast?”
“He surrendered,” was all Lloyd said. I got nothing more out of him.
These experiences with my teacher and mentor Lloyd were exciting, and maddening. I couldn’t understand a lot of what he was talking about at the time. I was only 20, after all, and my life experience was limited. But somehow I learned enough to use as the foundation to grow on my own over the years.
The drum was a curiosity and the soothing patter drew listeners in, shifting their awareness from the anxiety and aggression they were displaying while allowing their brain to entrain to the rhythms and into a calmer state (I talked about entrainment in Chapter 5 and about calm in Chapter 9). In both Ty’s and Charlie’s cases, calm occurred within a few minutes.
While I played for Charlie, Kathleen, the home’s director, came out and watched me play. I walked over to her after I finished, and we talked as we meandered through the gardens.
“Charlie, the man you just played for, is the aggressive guy I told you about on the phone,” she described. “He’s a sweet guy at heart, but we’ve been having three or four violent outbursts a week where someone is injured.”
“That’s a lot,” I said. “How badly are people hurt?”
“Not too bad, but we have to report them and we’re getting pressure to find him a different home if we can’t reduce the incidents. We’ve tried different medications and behavioral interventions, but nothing has really helped.”
“Do you know what triggers his aggression?”
“Most of the time it’s when he’s asked to do a chore that he doesn’t want to do. Other times he gets in one of the other guy’s [resident’s] faces. It’s worse during mealtimes. We have to work hard to manage everyone while they eat. Dinner is the most stressful time of day here.”
Kathleen described that Charlie has lived in a group home situation since he was 14-years-old. He was placed there due to his family’s inability to care for him and manage his anxiety and aggressive outbursts. This facility was his fifth group home.
Due to his non-compliance and severe behavioral reactions, Charlie was not involved in many of the day-to-day activities that the other residents enjoyed. The staff reported that he did enjoy riding and brushing the horses; but they didn’t allow him to do these activities often, due to his tendency to spontaneously hit the horse with a closed fist.
Aside from these aggressive behaviors, Kathleen described that Charlie’s anxiety also manifested in the form of self-stimulatory vocalizations and sleeplessness. The vocalizations were often threatening in nature, but there didn’t seem to be a correlation between his threats and his aggressive actions.
“His yelling and swearing seems to be a release mechanism for him,” said Kathleen.
“It sure is disconcerting, though,” I added. “When I first heard him, I thought he had Tourette’s.”
“No, he has autism.”
Tourette syndrome is a condition characterized by involuntary repetitive physical or vocal tics (Chapter 11 has more on Tics). Charlie’s verbal threats weren’t the result of Tourette syndrome, because his vocalizations contained form and more closely resembled perseveration (the repetition of an action, word or phrase in the absence of a related stimulus). Perseveration is a common trait of autism and is an area where I tend to see marked gains; I was eager to see if reducing Charlie’s anxiety would improve this behavior.
Charlie could speak clearly with excellent grammar and vocabulary, but he only talked in an aggressive manner. The fact that he could speak and had a vocabulary, albeit a nasty one, suggested that if I could reduce his anxiety, he may become more conversational in his speech. This wasn’t a primary goal in working with Charlie, but it was one area I intended to keep an eye on as he used his REI recording. As in the case of Jim, who I discussed in Chapter 14, I have seen the spontaneous initiation of speech occur in adults with autism as a result of reducing anxiety.
Kathleen and I talked for a couple of hours, going over the details of the study I would conduct. The plan was to create a custom-made recording for each of the residents. Each recording would focus on areas of concern specific to each resident. I would also attempt to reduce the overall level of aggression and anxiety in the facility.
You can order the book here